All You Need to Know About the Nursing Metaparadigms
Introduction
You may have heard the term “nursing Metaparadigm” thrown around, but you’re not quite sure what it means. In short, it’s a framework for nursing theory that includes three main pillars: nursing philosophy, research, and experience.
The Nursing Metaparadigm can help guide nursing practice in hospitals, other health care settings, and at home with patients and their families. Read on to learn more about the definition of a Nursing Metaparadigm, why nurses need to understand this concept, and how they use it daily. However, should you chose to skip this guide, our premium nursing writers are ready to cover you by handling that nursing assignment for you. All you need to do is placing an order with us!
What is the Nursing Metaparadigm?
The nursing metaparadigm is a set of beliefs that guide the practice and care of patients.
The metaparadigm is a conceptual framework or an idea-map about how something works. It can be used for purposes such as teaching (to explain things), research (to understand them), and decision making (what to do next).
The concept comprises two aspects: paradigm shift and paradigmatic thinking. Paradigm is the dominant theory within one’s discipline at any given time. In contrast, paradigm shifts are changes in fundamental ways of thinking, which result from new assumptions being adopted by practitioners over years of experience.
The nursing Metaparadigm includes six guiding principles:
- Caring, concern for life, continuity of personhood
- Wholeness in health/illness
- Relief from suffering
- Reverence for life to death continuum
- Safety principle with priority on patient’s well-being first
The nursing metaparadigm is about human beings [human being – an individual] as they exist in their culture. The nurse assumes responsibility for restoring broken connections between each person and his world.
A humanistic perspective values personality differences among individuals and emphasizes the uniqueness and dignity of every person.
Why is the Nursing Metaparadigm Important?
- The nursing metaparadigm creates a perfect foundation for nursing practice.
- The nursing metaparadigm is a key theoretical framework of nursing that establishes the beliefs, principles, and knowledge about human beings related to health, disease prevention, and healing practices.
- The paradigm addresses needs at all levels, individuals, families, communities, and social structures like economics or religion.
- It guides how nurses should think about themselves within their profession and with other professionals providing care.
Nurses use these guiding thoughts to inform decisions made during assessments (taking note of patients’ values), treatments (considering cultural differences), and evaluating outcomes (focusing on physical rather than just mental well-being).
You may also check nursing mnemonics
Nursing Practice


The nursing practice is the actual hands-on work of an individual or group that nurses. The nursing practice focuses on care, treatment, and rehabilitation for injured, ill, or living with a chronic condition such as dementia.
Nursing theory is the study of nursing methods, including diagnosis, prognosis, prevention, and outcomes, to provide information about patient management.
The human beings section addresses how humans will change over time in terms of physiology (having better health), behavior (becoming less aggressive), and cognition (improving memory).
The nursing profession is the nursing specialty that deals with the health and wellness of people.
A nursing Metaparadigm provides nurses with knowledge on what it means to practice nursing in today’s society–its theories, concepts, and approaches,
What are Nursing Theories?
Nursing theories are the way to understand nursing and the world. These theories are developed in response to healthcare changes, technology advances, or new developments within a profession.
Each of the nursing theories helps practitioners do their job better by providing them with an understanding of what they are doing and how it affects patient outcomes.
In nursing education, one must study nursing theories to understand the underlying concepts and principles that guide a nurse’s practice.
The Nursing Metaparadigm theory is one of many theories used in nursing education, but it is also important outside academia. This theory has been developed over time by nurses themselves with input from clinicians and other health care professionals to help practitioners at all levels make more informed decisions about their everyday work while caring for patients.
The goal of this nursing metaparadigm is to change or improve healthcare delivery systems and make sure each person who comes into contact with a patient can provide them optimal outcomes through individualized attention and personalized caregiving methods.
You may also check nursing diagnosis for UTIs
Defining Terms in Nursing Theory
Philosophy: A theory of knowledge.
Metaparadigm: A general model that transcends disciplinary boundaries and provides a framework for understanding phenomena in their relation to each other.
Nursing Metaparadigm: The nursing metaparadigm is the overarching theoretical perspective shared by professional nurses encompassing all aspects of nursing practice, including its historical roots, major concepts, research findings, and theories from various disciplines applied within clinical care settings, as well as its future direction.
Theory: A model of something observed in nature or society; the branch of knowledge concerned with theories and their principles.
Nursing theory: It refers to the mental schema nursing professionals use as they practice professional nursing.
Concept: It refers to the fundamental ideas or the generalized concepts used to construct a theory.
Nursing research: It is a systematic effort to identify, analyze, or evaluate nursing phenomena and processes to generate new knowledge for nursing practice and education.
Nurse practitioner: A professional nurse who practices as an autonomous health care provider of direct patient care with specific credentials for advanced generalist practice. NP’s provide services such as diagnosis; treatment planning; counseling on nutrition, medications, lifestyle issues, etc.; collaboration with other physicians; minor surgery duties; monitoring patients during treatments like chemotherapy or dialysis and many others.
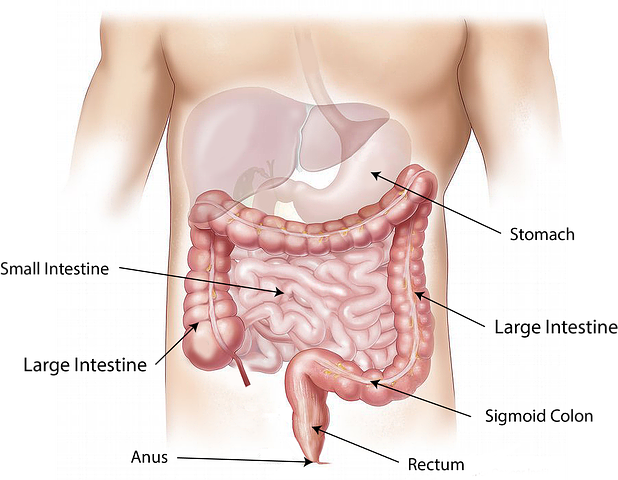
Body systems: This refers to the various systems of the body, such as skeletal, muscular, and nervous.
Brain: The center for consciousness or awareness in humans and other mammals (for example, rats) located within the head between two protective membranes called hemispheres. The left hemisphere is associated with logical thinking. In contrast, the right hemisphere is more creative.
Cardiovascular system: A system consisting of a network of blood vessels that carry blood to all parts of an animal’s body.
Circulatory system: “The process by which nutrients are transported through vascular plants from roots to shoots and leaves.”
Differential diagnosis: This involves identifying those factors that differentiate among possible causes to plan appropriate treatment. It may also involve differentiating among diseases with similar symptoms but differing effects.
Human beings: An individual human person who can be identified by any one of his/her distinguishing characteristics (including appearance).
You may also check nursing diagnosis for pulmonary edema
History of Nursing Theories
The history of nursing theories is quite interesting. The history of nursing theories goes back to a time before modern medicine was discovered and practiced. Then, the nurse had more responsibilities than just taking care of patients with different illnesses or injuries. Evidence from ancient Egyptian tombs showed that there were many nursing tasks and caring for their patients’ physical well-being.
There are usually three types of nurses: generalist, specialist, and advanced practice clinicians who may have experience as a registered nurse (RN) and licensed practical nurse (LPN). They all provide different levels of patient care depending on the specialization they have chosen among themselves, such as mental health/substance abuse counselor, pediatrician, gerontologist, or psychiatric technician.
Nurses can choose from various nursing specialties to specialize in, such as neonatal, oncology, or pediatric nurses.
Nurses are also responsible for the tasks before and after surgery that helps prepare patients physically and mentally. For example, for an upcoming operation, they can give preoperative instructions about when to stop eating or drinking certain foods and advise them to take prescribed medications beforehand.
Nurses can also advise new mothers who might be planning another pregnancy following childbirth to ensure adequate spacing between pregnancies to avoid complications during delivery.
Human beings have always needed care from others since their first day of life because caring is necessary for survival (or well-being). This need will never go away so long as human beings exist.
If you’re a college student, you may be interested in nursing diagnosis for nausea
The Nursing Metaparadigm


The nursing meta paradigm focuses on the care of human beings.
The nursing meta paradigm is grounded in the nurse-patient relationship, and it’s a wisdom-based practice that emphasizes cooperation between healthcare professionals and patients. It aims to promote health care and wellness for all people without discrimination or disparity.
It was developed by Margaret Morgan, who believed that nurses “must not only be aware of our own strengths but also recognize where we have weaknesses.”
This framework acknowledges the way individuals live with chronic illness on every level: body, mind, spirit, and how they cope with an ever-changing environment. In addition, it recognizes the diversity of cultures that shapes beliefs about life processes, death, spirituality, and morality.
Person
The term person in nursing is used to describe the holistic, individual being. The person includes their body and mind as they interact with each other in a social world.
The term also can be used for those who are not yet born or have died because nurses need to understand how all aspects of a human’s life affect that person when they enter into care.
Environment
The environment in nursing means all the things in a person’s world. This includes physical and social environments as well as the natural environment.
The nurse must focus on these aspects of care because they are all interconnected, meaning that one can impact another or affect how it will be experienced by the individual being cared for.
Health
Health refers to the many aspects of a person that are important to well-being. They include physical, mental, spiritual, and social health and the natural environment we live or work in.
The nurse’s job is to focus on all these aspects when caring for a person to have an overarching view of them holistically and not just one aspect at a time.
Nursing
The phrase nursing meta paradigm has been around in the nursing field for decades and references an overall worldview.
It can help nurses see connections between many aspects of care so they can broaden their focus when caring for clients.”
You may also check nursing diagnosis for diarrhoea
Components of Nursing Theories
For a theory to be termed a nursing theory, it must involve the following three components:
– a set of concepts or principles that are used to guide practice
– an underlying philosophy about people and their environment
– a process for addressing problems in care. (Throckmorton)
Phenomenon
The word Phenomena refers to any condition of existence or appearance, whether external or internal. It also refers to anything happening outside one’s conscious control (Merriam-Webster Dictionary). This includes perceived sensations such as colour, sound, taste, and touch, including thoughts not directly experienced through sense organs.
In nursing practice, it is important to recognize the phenomenon of human beings providing nursing care. There are different theories that nurses must use when providing care, and it is difficult for a nurse not to practice a certain theory because they all have their unique way of how it should be used. Theories can vary from person-centred or family-centred, directly affecting the patient’s experience with being cared for by a nurse (Throckmorton).
Concepts
In the nursing profession, the term concept means understanding the meaning of something and having mastery over it. Concepts are also important for nursing practice because they provide a foundation for nurses to build their knowledge on specific topics or theories.
Definitions
Definitions are a set of words that are used to identify the meaning or significance of something. Definitions can be found in textbooks, dictionaries, or medical websites where patients can learn more about their conditions and treatments.
Students must understand the medical terminology and the definitions of body parts, diseases, treatments, symptoms, etc., to help them with their nursing studies.
Relational Statements
The term relational statements are often used to describe nursing’s focus on caring for the whole person, considering their social and environmental context and physical needs.
Nurses are taught that health is not a state of being; it is a process involving all aspects of life. This approach to care recognizes the relationships between people or groups and the relationship between people’s lifestyles (including their diet, activity level, and work/sleep habits) with their health.
Assumptions
When dealing with patients, there are various assumptions that nurses make. These assumptions are based on the model that there is a problem with the physical body, and it has to be fixed by medical professionals such as doctors or nurses.
For example, if someone came into the hospital complaining of chest pain, they would automatically assume that there may be a problem with the heart and begin checking for blood pressure issues or heart rate changes.
You may also be interested in nursing diagnosis and care plan for Insomnia
Why are Nursing Theories Important?
The knowledge provided by nursing theories is essential for nursing students, as it provides them with a framework and tools to process information.
It is also essential to guide future practice so that nurses will use this knowledge to make decisions about how they work with their patients.
In Profession
Nurses can also use their understanding of human beings for decision-making regarding diagnosis and treatment plans, interventions, and treatments because people make up who we are. Thus, a nurse cannot be an expert practitioner in health promotion and prevention but does not know how humans work or motivate them (Dolan).
The theory provides nurses with the tools they need to guide their decision-making process to be done more efficiently without making any mistakes along the way.
Nursing theories help people think about various situations and how they might affect an individual’s health status, relationships with others, interactions within society, and other aspects of life. It also helps nurses explain why decisions were made when working on patients’ conditions, from diagnosis through treatment to recovery back into society again.
Why are Nursing Theories Important In Academic Discipline?
The nursing theory provides students with the knowledge to identify the issues and assess and plan interventions to resolve them. The theory is a map or set of guidelines for nursing practice.
The knowledge provided by these theories helps equip students of nursing intellectually, morally, and spiritually.
Nursing theory helps students understand the complexities of human life.
Nursing theory provides students with a language to talk about and study their work and provides them with guidance on how they should approach caring for patients.
In the nursing profession, one is required to understand the nursing metaparadigms, which is the “overarching theory that guides decisions about nursing practice.”
At their core, the human being has spirituality, and part of nursing care includes attending to this spirit in patients.
When students study these theories, they can understand spiritual growth as well as physical healing.
You may also check nursing diagnosis and interventions for Diverticulitis
Why are Nursing Theories Important In Research?
Nurses need to know and understand a variety of different theories that guide their research. This includes the following theories: feminist, constructivist, postmodernist, phenomenological, cultural relativism, and others.
These various perspectives help in developing an understanding of illness from many angles. Nursing Theories are also important because they can inform nursing practices by helping practitioners explore their own beliefs or attitudes towards certain topics while still maintaining a neutral stance on these issues themselves(Smyth). By doing so, we can better serve our patients, who will likely have very different opinions and ideas than ours.
Classification of Nursing Theories


Nursing theories are classified according to two major categories: the philosophical approach and the tradition of practice. The three main traditions are scientific, humanistic (or existential), and postmodern/poststructuralist.
By Abstraction
An abstraction is an approach that considers the nursing metaparadigm as a set of models, theories, principles, and hypotheses for describing phenomena in health care.
The three major categories are based on philosophical approaches to nursing: scientific, humanistic (or existential), and postmodern/poststructuralist.
Grand Nursing Theories
-Grand nursing theories are high-level theories that have been used by nursing for a long time.
-They are generally based on one of the following assumptions:
Theory A assumes life is not fixed and determined, so human beings can change according to how they respond to their environment.
Theory B assumes life has no meaning, but rather it’s a result of chance or necessity.
Theory C assumes life has an inherent purposeful design, meaning, and value regardless of what happens in our lives.
Middle-Range Nursing Theories
Middle-range theories in nursing are more limited in scope and are used to explore the complexities of a certain topic.
In contrast, long-range nursing theories encompass all aspects of a specific phenomenon and can be more expansive.
Middle-range theories identify main concepts related to human beings or health care providers as they work with patients with complex needs such as chronic diseases.
Practice-Level Nursing Theories
Practice-level nursing theories are defined as the nursing theories usually applied to a given discipline’s practice. Practice-level theories do not have universal acceptance, and research findings or other arguments can challenge them.
The practice-level theory is often called “clinical judgement.“
Clinical judgments at the practice level meet the needs of individual patients. However, they may not meet all patient’s needs as there is no set standard for what constitutes an acceptable clinical decision. For instance, some nurses would consider using intravenous fluids in this situation while others might not because they believe that containing fluid loss through replacement with electrolytes orally will suffice.
The nurse must weigh their own experience and knowledge against the best evidence when making these decisions.
By Goal Orientation
Theories can also be classified based on their goals. They can be descriptive or prescriptive.
Descriptive Theories
Descriptive theories in nursing are theories that are meant to describe and analyze nursing practice.
Descriptive theory in nursing is studied to understand the meanings, symbols, patterns, and structures of a particular phenomenon or experience.
There are two types of descriptive theories: factor-isolating theory and explanatory theory.
Factor -Isolating Theory
The factor isolating theory states that the experience of the physical self is experienced through the senses. In this theory, a person’s physical self is not an objective reality; instead, it can be created from memories and perception.
The factor of isolating theory views that the self-concept in a person is shaped by his experiences with other people, such as family members or friends. It states that one interacts more readily with those who share similar personality traits, usually based on race, gender identity, sexual orientation, etc. This perspective of the human being makes one view him/herself as dependent upon others to form their sense of individuality.
This type also considers how living conditions affect personal interactions among individuals and groups, particularly at home, where there may be considerable social inequality influenced by wealth distribution and social factors.
Explanatory theory
The explanatory states that self-concept is a result of people’s perceptions and judgments about themselves.
The self in an explanatory theory views him/herself as being independent of the thoughts and feelings of others.
This perspective also views each person’s self-identity as stable and consistent over time, which they believe to be shaped by their accomplishments rather than those who have influenced them or helped shape them. Thus, this type allows for individuality but does not consider how other human beings may affect this sense of independence that constitutes one’s self-concept.
Explanatory theories focus on exploring individual needs with little attention paid to social interactions among individuals or groups. As a result, theories such as these tend to focus more on personal development than interpersonal relationships.
Prescriptive theories
Prescriptive theories offer guidance for action by prescribing how nurses should behave with patients and other people involved in healthcare delivery (including health professionals such as physicians). The prescription includes suggestions about which interventions work best when they should be used, and why they produce better outcomes than alternative approaches; it will include information about ethical responsibilities in relation to autonomy issues such as informed consent activities, among others.
You may also check nursing diagnosis and care plan for hypovolemic shock
Other Ways of Classifying Nursing Theories
There exist different ways of classifying nursing theories.
The classification of these theories ranges from content, process, and discipline to the philosophical perspective that they encompass.
There are other ways to classify these nursing theories, such as whether they have use in clinical practice or not.
These methods of classifying nursing theory should be used when trying to understand their differences and similarities, so knowing how each one functions helps solve different problems about caring for people.
Classification According to Meleis
Meleis was a nurse theorist.
According to her, there are three ways of classifying nursing theories: according to content, process and discipline, and finally, the philosophical perspective encompassed by them.
The difference between a theory is whether it has been used in clinical practice or not.
For example, if we consider those that have no use but still serve as an intellectual pursuit, they would be classified as philosophy. However, if they have some usage in clinical work with patients, they would fall under either one or both of the other two types.
Need-Based Theories
Need-based theories are the types of theories based on the need for care and best suited to meet those needs.
The nursing care would be structured around meeting these needs in different ways instead of using a specific philosophy, process, or content.
Interaction Theories
Interaction theories are another way of classifying nursing theories.
A theory in this classification is either focused on the individual or more encompassing to include a person’s environment.
The focus of these interactions can range from action, cognition, feeling, or behaviour.
This way of categorizing nursing theory helps to understand how each one operates and their differences, which help solve different problems that people encounter during care.
Outcome Theories
Outcome theories involve understanding the goals and outcomes of a patient’s health care.
An outcome theory is determined by what ends the person wants to achieve, which can be physical or psychological in nature.
The main goal of an outcome theory is to see whether it achieved its desired effect on that individual.
Outcome theories are often used to categorize nursing theories because they focus on how well a nurse was able to provide care with their knowledge and skill set.
Psychosocial Theories
Psychosocial Theories involve understanding human relationships.
A psychosocial theory considers not only a caregiver but also an individual’s social setting, including family and friends.
This type of classification helps nurses understand what a patient’s needs are and provide care accordingly.
The psychosocial nursing theory is based on how well a nurse can provide patients with their desired outcomes, which can be physical or psychological.
Determined by the ends that person wants to achieve, it can either be physical or psychological. For example, outcomes may include pain relief, symptom control, health promotion, etc. The goal of an outcome theory is to make sure it achieves its desired effect.
List of Nursing Theories and Theorists
Many theorists in the nursing field have come up with different theories to help guide the nursing profession.
Florence Nightingale
Founder of Modern Nursing and Pioneer of Environmental Theory.
“Nightingale pioneered modern nursing and was a key figure in shaping the field of professional nursing.” She created “the science for keeping clean, personal hygiene, how to dress wounds.”
She also pioneered nursing education that emphasized bedside care. Her work established an essential foundation for hospital management then and now. The second edition of her book appeared posthumously with corrections made by her sister Parthenope who also published two other editions after she died.
Also, check C diff smell and diagnosis
Ignacio Garcia Pineles
Ignacio Garcia Pineles (1809 – 1841) is often called one of the fathers of modern medicine because he introduced humanitarian principles into medical practice, which were not accepted until much later.
He advocated humane treatment of the mentally ill and condemned the use of torture. He was also a pioneer in occupational therapy, which served as an important precursor to physical therapy.
Hildegard E. Peplau
She pioneered the theory of the caregiving relationship in nursing.
She conceptualized the human being as holistic and psychosocial, not just physical or mental.
Her theory was a paradigm shift from traditional biomedical practice, which focused on treating body systems independently. Instead of treating symptoms, she looked at patients holistically, emphasizing promoting well-being through social interactions with others (Peplau et al., 2014.)
Virginia Henderson
She developed the theory of “nursing as natural care,” which is a nursing metaparadigm. Henderson believed that human beings are born with an innate tendency to grow and heal but require the help of others (including nurses) for this process to happen.
She also introduced concepts such as “focusing on wholeness,” and recognizing individuality. In addition, she encouraged nurses to use their intuition when caring for patients instead of following set rules or orders from doctors.
The theory was highly influential at the time it was created. However, its popularity has declined due to changes in healthcare.
Faye Glenn Abdellah
Developed the 21 Nursing Problems Theory
He came up with the idea to write his first book, “The Nursing Metaparadigm: Definition and Practice,” in the early 1990s. He explained that this nursing theory is not a new idea or concept but has been around for many years.
It was just March of 2012 when he finally published it, which he said felt like one of the best days ever.
Faye Glenn Abdellah never thought that this day would come because he spent so much time finding out about the ideas behind it all these years. But now, by publishing “The Nursing Metaparadigm: Definition and Practice,” Faye Glenn Abdellah can share what he learned over 20 years ago with others who are interested in helping others heal themselves by using human value practices.
Ernestine Wiedenbach
Developed The Helping Art of Clinical Nursing conceptual model.
Wiedenbach’s three values are the spiritual, humanistic, and scientific worldviews used to define nursing care practices for her Roper Hospital nurses at Duke University Medical Center.
The nurse is an individual who believes in a spiritual world where there is equality of all people with equal rights before God. They believe that health should be promoted using science and medical knowledge with compassion by respecting each person as a whole.
They also have an unconditional commitment to providing compassionate care regardless of age, gender, or race.
The nurse must integrate this into their practice on both physical/biological levels (science) and psychosocial aspects of illness (humanistic).
This definition emphasizes how much thought Ernestine gave to the underlying spiritual values that guided her nursing practice and how they differed from other models of care.
The nurse believes in a spiritual world where there is equality of all people with equal rights before God;
They have an unconditional commitment to providing compassionate care regardless of age, gender, or race.
You may also check nursing interventions for heart failure
Lydia E. Hall
Developed the Care, Cure, Core Theory is also known as the “Three Cs of Lydia Hall.
She came up with the nursing Metaparadigm, and through her research, she discovered that human beings are complex organisms. She also found out that we can’t just rely on the clinical ability to solve patients’ problems. Instead, nurses need to understand their true nature.
In her theory, she cited that nurses should accept the complex nature of human beings and be aware that there are many values to consider when treating them.
She also said nurses need to understand their true nature. They must respect patients as individuals, care for their needs, and figure out what they want from their nursing experience.
Nurses can learn more by exploring the philosophy behind clinical decision-making using her theory.
Joyce Travelbee
The human beings’ ability and joy for learning (their “clinical” experience) have greatly influenced her definition of nursing and what nurses do in clinical practice.
In her Human-to-Human Relationship Model, she quotes Arine C. King, RN, and author of the book “The Nursing Metaparadigm,” who states:
“Nurses are not simply clinical practitioners who attend to human beings as if they were inanimate objects; rather nurses understand that human life has a sacred dimension.”
In her first nursing memoir, she wrote about how important it is for nurses to use their God-given talents by caring for those around them with an open heart.
She felt so strongly about this that when asked what was most important to remember before going to work each day, she would always say, “Stick your finger in somebody’s blood!” She wanted nurses to feel the power of touch – something we often forget as technology advances and does more things without us physically being in touch.
Kathryn E. Barnard
She developed the famous Child Health Assessment Model, which states that children will need a different type of care depending on whether they are healthy, sick, or injured.
She stated that children need to be assessed differently and that the nurse needs to know what type of care is needed.
Evelyn Adam
- Focuses on the development of models and theories on the concept of nursing. She states that nursing is a humanistic practice.
- She defines the nursing Metaparadigm as “a set of assumptions which provide an organizing framework for thinking and acting within nursing.”
- The philosophy behind this concept implies that nurses are neither passive recipients nor providers of care. Still, rather participants in creating health, even when they may not be present at the moment, it occurs. They must always keep health promotion and prevention goals in mind while treating patients to ensure long-term wellness.
- Adam proposes that models should be revisioned by adding new factors or variables to give them more validity to contemporary life events such as a postmodern world (which has been developed since her writing).
As a nursing student, you may also be interested in nursing diagnosis for Fluid Volume Deficit
Roper, Logan, and Tierney
They developed A Model for Nursing Based on a Model of Living. It states that the nurse’s role is to help the individual life as fully and productively as possible. The nurse does this by focusing on the person’s needs, not just their symptoms or medical diagnosis. They believe that nursing should be a holistic approach to health care that focuses on prevention, wellness, treatment, and rehabilitation.
The model defines five dimensions:
- Physical self-concept
- Emotional well-being
- Interpersonal relations with others (social network)
- Intellectual functioning
- Spiritual beliefs about one’s life with God/ultimate reality
Roper et al. describe these dimensions as “an integrative framework for all human activity.” Nursing practice includes understanding how each dimension affects every other dimension, which then affects health outcomes throughout an entire lifetime.
Ida Jean Orlando
She developed the nursing processing theory. Her theory stated that nursing is an art, science, and profession.
She believed that nurses should be caring in all three aspects.
She also thought nursing was a craft because you have to employ skills like diplomacy when communicating with patients or family members about treatment plans that can’t always go according to plan.
The theory encourages nurses to use their creativity and wisdom while executing clinical care. It allows for flexibility during unpredictable moments to respond appropriately without having rigid guidelines set on them.
Jean Watson
She pioneered the Philosophy and Theory of Transpersonal Caring. Jean cited that there are four themes of the theory;
- Understanding that human beings are a part of nature; they belong to themselves and others.
- Recognizing the uniqueness of each individual, from whence come their individuality and creativity.
- Seeing human beings in contexts that have never been considered before, for example, seeing them as “futures” instead of just “present.”
- Taking responsibility for one’s own healing (internal), such as through education or psychotherapy, emphasizes selfhood rather than charity care.
You may also check nursing diagnosis for Osteomyelitis
Marilyn Anne Ray
Developed the Theory of Bureaucratic Caring.
She stated that bureaucratic caring is the nurse’s responsibility to provide care and services that meet this population’s shared needs.
Ray also states in her theory, “There are three major sources from which we derive our sense of self-worth: esteem derived from living up to what we believe society expects us to be; dignity derived from feeling ourselves needed by those who depend on us or whom we need for survival purposes; and personal worth derived from feelings of accomplishment.”
The Theory argues against doing all the tasks because there can never be a person who will do everything well enough. An individual cannot have complete knowledge of medicine today. Thus, hospitals should hire nurses with diverse backgrounds so they can meet all the patient’s needs.
Patricia Benner
Caring, Clinical Wisdom, and Ethics in Nursing Practice
Patricia believed that caring is an essential component of nursing.
Patricia believed that clinical wisdom was a way to explore the complexities of nurses and patients in caring for each other.
Patricia’s definition of ethics involves doing what you believe is right, even when following guidelines set out by legislative bodies like law or legislation might lead you down another path.
A nurse’s work entails balancing many different options: physical needs versus emotional needs; pain control versus anxiety reduction; healing environment versus cost containment; discharge against admission; symptom relief against prevention—to mention but a few examples. This requires making tough decisions while being responsive to shifting priorities and circumstances as they arise during caregiving activities with individual clients, families, and groups on the unit.
Kari Martinsen


Founded the philosophy of caring. Knew that the healing process begins with caring for oneself.
Felt compelled to find a way of understanding and living one’s life, rather than accumulating knowledge just for its own sake.
Martinsen was convinced that this need could not be fulfilled by taking refuge in traditional disciplines such as art or science alone; rather, it required integrating various elements from many different fields, including medicine, psychology, sociology, economics, anthropology, and theology.
You may also check nursing care plans
Katie Eriksson
Katie developed the Theory of Caratative Caring
- The theory of caritative caring is based on the idea of healing.
- is a process of empowerment and that it starts by acknowledging.
- It is validating and affirms people’s feelings.
- The nursing model believes that all human beings are inherently good but have been hurt in some way or other.
- Healing for this theory comes from helping others heal themselves. This theory has four main components: emotional needs, cognitive needs, physical needs, and spiritual well-being. For instance, if someone were to get burned, we would care for them emotionally first, then go about dressing their wound or doing whatever else necessary to help with their pain levels, and finally check they had access to psychosocial support services so they could be cared for spiritually as well.
Myra Estrin Levine
She developed the conservation model, which was Vineyard Hospital.
She developed the conservation model to provide a framework for human beings facing illness, suffering, and death.
The Levine Method is an approach to end-of-life care that is administered by her team of nurses at Martha’s Vineyard Hospital in Massachusetts. The method acknowledges that patients recover from emotional trauma through their experience of love and intimacy with others and supports them on their journey as they die.
This process usually takes place over several days or weeks, where families have opportunities to reconnect with each other. It also provides caregivers with the opportunity to engage in meaningful work, which typically involves holding hands, talking softly, and singing together while sitting close enough so the patient can feel our presence but not see it.
Martha E. Rogers
She developed the theory of unitary human beings.
- In Roger’s Theory of Human Beings, she defined Nursing as “an art and science that is humanistic and humanitarian.”
- Rogers considered nursing to be a holistic and person-centred approach.
- She believed that all problems in the human body are related; therefore, providing one way of treating any illness is better than using different treatments for each symptom.
- The goal of this theoretical framework was to create an environment where nurses could improve their ability to care for patients holistically while maintaining ethical standards through direct interaction with them.
Dorothea E. Orem
Founded the self-care theory, which is a holistic theory of nursing.
Orem believed that nurses should provide care for the patient, themselves, and their families to promote self-healing.
She also argued that society’s view of healthcare providers was among the reasons not enough Americans seek medical attention when they need it; she wanted to change this by shifting focus on health promotion rather than diagnosis or treatment only.
As a nursing student, you may be interested in nursing diagnosis for GERD
Anne Boykin and Savina O. Schoenhofer
- The Theory of Nursing as Caring: A Model for Transforming Practice
- This theory is a comprehensive theory of nursing that describes the nature and role of caring in health care.
- The theory defines caring as a process and activity with four major components: perspective, assessment, intervention, and evaluation.
- Nursing Practice -Provide physical comfort to patients by fulfilling their basic needs for food, water, warmth/coolness, etc.; prepare them for surgery; provide emotional support through communication or touch; assist doctors during procedures such as examinations or treatments; monitor patient’s progress post-surgery via blood pressure measurements, or other means to detect complications early on.
Afaf Ibrahim Meleis
Transitions Theory
Afaf cited that transitions theory incorporates the following theories: Social Cognitive Theory, Emotional Regulation Model, and Mindfulness
Transitions can be any type of change in a person’s life. This includes changes that happen over time as we age or even sudden events such as death.
Transitions affect our mental health because they are part of living.
Transitions Theory is based on nursing meta paradigm history when Barbara Zinn first introduced it in her paper “The Nursing Process: A Paradigmatic Perspective,” which she published in 1984 to describe what caring looked like for nurses during this period when there was no set way to practice nursing except to do whatever
Nola J. Pender
Founded the health promotion model.
It focuses on improving the wellness of populations, communities, and individuals.
Developed health promotion interventions to promote healthier lifestyles in a range of settings.
Nola J. Pender’s History – nurse educator who was instrumental in developing nursing education curricula for public schools; published “Healthy People: A Practical Guide” (1974), which became an influential primer on epidemiology and population science that has been translated into 12 languages.
Madeleine M. Leininger
Founded the Culture Care Theory of Diversity and Universality
The study focuses on the differences and similarities of human beings.
It is used as a guideline for nursing care when people encounter cultural beliefs or practices different from their own.
Madeleine Leininger’s History – nurse educator who published “Cultural Care: A Theory of Diversity in Nursing Practice” (1985), which became an influential text on diversity
You may also check nursing diagnosis for cystic fibrosis
Gail Lynne Goodwin, PhD
Founded the Epistemological Contextual Model of Health and Illness Paradigm.
The study focuses on how humans experience health and illness in context with society, culture, and nature.
Gail Lynne Goodwin’s History – Nurse educator who developed contextual models to explore clinical reasoning within social science frameworks.
Margaret A. Newman
She founded the Health as Expanding Consciousness model.
She believed that people need to be aware of their health and that they have the power to change it
Margaret A. Newman’s History – Nurse educator who developed models for caregiving.
You may also check nursing research topics
Beverly Potter, PhD
She founded the Empowerment Model, which is focused on individual responsibility for wellness concerning society, culture, nature, and self-care. Beverly Potter’s History – she is a nurse educator whose work focuses on empowering individuals with chronic illness through education about themselves as a person living with severe diseases or long-term conditions.; published “Nursing: Caring For The Person In Context” (2000)
Carol Ann Tomlinson-Keasey
She founded the Health/Illness Continuum model representing how personal choices can positively affect one’s health.
She developed the Health Promotion Model for nursing practice, focusing on wellness, rehabilitation, and enabling people to return to maximum functioning in society.
Ramona T. Mercer
Maternal Role Attainment—Becoming a Mother
-She believed in caring for the whole person.
-She became a mother at age 36 and felt that she was now in the best position to “understand what maternal nurturing meant.”
She published “A Mother’s Cross—Dorothea McDonagh” in (1972)
-The author found it difficult as a new wife, daughter, and mother. She feared her identity would be lost or submerged by these roles.
She had also been an excellent student who loved school work but hated exams because they always seemed very stressful. This made her want to quit being a nurse altogether after graduation from nursing school; this decision was changed when Dr. Robert Sibbald urged her not to give up on herself so easily.
Pamela G. Reed
Self-Transcendence Theory
Pamela stated that she was not a natural healer, but she had good instincts and intuition.
She said that the patients needed to know their family and friends loved them.
At first, Pamela felt guilty because she didn’t feel like she was giving her patients what they wanted or needed from her as a nurse; later on in her career, though, she realized it is important for nurses to be compassionate with themselves, too, which can help them heal better.
Pamela then went on to say that this theory assumes “that all human beings have an innate capacity for self-healing.” She also explained how the art of healing included being kinder than necessary – such as saying ‘please’ when asking somebody to do something.
You may also check nursing diagnosis and care plan for appendicitis
Carolyn L. Wiener and Marylin J. Dodd
Theory of Illness Trajectory
The illness trajectory theory is a nursing metaparadigm that helps nurses understand getting and staying well. The approach is based on three things: That is:
The caregiver does help a person get well, stay healthy, or manage their symptoms.
– How people change over time with chronic illness and how they adapt to changes that occur during an episode of acute illness; and
-How caregivers influence this process through interactions with patients (Cuddy).
Georgene Gaskill Eakes, Mary Lermann Burke, and Margaret A. Hainsworth
Theory of Chronic Sorrow
-The chronic sorrow theory is a nursing metaparadigm developed to help nurses understand how illness might impact an individual.
-The theory of chronic sorrow helps us understand the response to grief and death based on different stages in life.
-People may experience varying degrees of sadness depending on their age, and this theory can be used as a guide for caring practices during these periods.
You may also check nursing diagnosis for metabolic alkalosis
Elizabeth Kubler-Ross’s Stages of Grief Model
Kubler Ross’ model includes five stages: denial, anger, bargaining, depression, and acceptance (also called resignation). However, this model has been criticized because people do not necessarily progress smoothly through all the steps, nor does everyone follow them to heal from loss or other issues.
Katharine Kolcaba
Theory of Comfort
The theory of comfort is based on the idea that by caring for someone in need, one can feel comforted and offer a sense of peace. In addition, the theory suggests that grieving people who have suffered trauma receive support from individuals (friends) with whom they trust and have an intimate relationship.
You now have the required knowledge about the nursing metaparadigm and its importance. You have also learned about different theorists and their impact on the nursing field. If you want more insight about this or looking for someone to help you with your nursing metaparadigm essay, contact us today.