Nursing Diagnosis & Intervention for Colostomy-Student Guide
Introduction
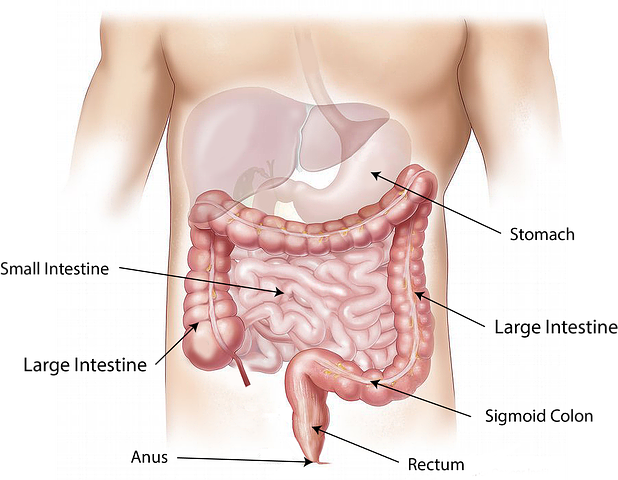
A colostomy is one of the surgical methods performed by a surgeon to remove some portion of the colon or intestine through the abdomen.
Colostomy can be temporary or permanent depending on the need of the patient. The primary purpose of a colostomy is to divert the flow of stool from an area that is diseased, injured or removed colon out of the body.
Colostomy can be done during proctocolectomy surgery, in which part of the sigmoid colon is removed and a stoma is created for waste evacuation. In this situation, a colostomy is temporary until the newly formed intestine is well enough to carry stool out of the body. A colostomy can be done only on one side of the colon as in ileostomy or on both sides, as in colostomy.
Colostomy can be done using two ways:
- Open surgery, which is also known as Laparotomy
- Laparoscopic, also known as keyhole surgery
Open surgery is where a large incision is made on the stomach to locate the colon.
Laparoscopic is preferred between the two procedures, is where small incisions are made on the tummy, and a camera is used to find the colon. The reason why this is preferred to open surgery is that the healing process is quicker. The risk of this procedure is also low because of two major reasons. One is the speed at which the patient heals. The second reason this procedure is preferred is that the pain experienced by the patient is less, although this procedure is costly.
As you read, keep in mind that our top writers are ready to help in case you get stuck or cannot complete your nursing assignment due to other reasons such as a busy schedule. All you need to is place an order with us!
Disclaimer: The information presented in this article is not medical advice; it is meant to act as a quick guide to nursing students, for learning purposes only, and should not be applied without an approved physician’s consent. Please consult a registered doctor in case you’re looking for medical advice.
Loop Colostomy
This procedure is usually used when the colostomy is temporary. This is because the procedure is easily reversible.
This creates an opening in the abdominal wall above the pelvic bone on one or both sides. The intestine is brought through this opening, and a bag is connected to collect faeces, which typically drain into the toilet.
Thorough colostomy (also called end stoma)
This involves cutting a hole in the skin that covers your abdomen near the belly button. A surgeon will then bring a loop of intestine out through the hole to create a stoma or opening. The opening is called an ostomy. If no part of your colon was removed, your healthcare provider might refer to this as a stoma ileostomy.
A loop colostomy is sutured in place with help from surgical staples. Through colostomy is held in place with surgical tape or a small adhesive bandage called an ostomy pouch.
The two most common types of colostomies are side and end ones. Both of them present the same complications to the patient, but one can be cured at home by specific dressing materials, which will be explained later in the article.
The treatment of a colostomy is a very delicate matter and requires a lot of patience from the patient in order to succeed.
The use of various materials such as dressing sheets, adhesive strips and elastic bandages are often required in order to keep feces away from the skin while the opening is healing and not infecting with harmful bacteria that can cause an odor.
The opening in the abdomen through which feces pass into a bag attached to the abdominal wall is called a stoma, and such patients are known as ostomates.
After surgery, the protruding part of your intestine or colon that exits out from your body is called a stoma. Over time, the stoma will become pink or red and form a hard ring of flesh around it called granulation tissue. The opening under your skin that is used for removing stool from your body is called an ostomy.
Your bowel movements after surgery are usually loose and watery. You will pass mucus, which is typically brown or clear in color.
A colostomy bag is a special device that collects stool from the stoma. It’s a pouch made of waterproof material worn outside your body that contains a small filter to catch any solid matter, so you don’t feel it and enjoy life as normal thanks to such a device.
Generally, a colostomy bag is placed conveniently on the patient’s body so an ostomate can freely move around without worrying about the placement of the pouch or leakage.
The surgery for colostomy is quite complex and extensive. It requires a team of surgeons to be performed within 6-8 hours, depending on the amount of intestine that needs to be removed. The long duration makes it uncomfortable for a patient.
Reasons for Colostomy
The colostomy is done in the following situations:
- A blockage of the intestines, which may be due to a tumor or congenital disorder
- Injury of the intestine that does not heal (intestinal ulcer) after blood supply is restored
- A serious infection that led to the end of gangrene or death of some part of the intestine
- Sigmoid colon cancer requires the removal of a large portion of the colon and rectum
- Surgery to control anus bleeding resulting from fistula in case of inflammatory bowel disease
- Surgical procedures done around the anus may result in injury or damage to the colon.
- Conditions that require removal of rectum and anus such as ulcerative colitis, proctitis and colon cancer
Risks of Colostomy
- Organ damage is among the other risks of colostomy. Damage can affect the small intestines, colon, anus and rectum, which results in incontinence or constant leakage of stool out from a new opening around the anus. The stool may have a foul odor that causes embarrassment to the patient.
- Breaking open of wounds around the anus, requiring re-surgery to close the opening
- A hernia may occur at the opening of the colon, causing the anus to nearly touch the ground.
- Constipation
- Gas in the colon or rectum that causes diarrhea
- Risk of impaired skin integrity, e.g pressure ulcer
- Infections around the wound either from fecal matter or blood
- Internal bleeding from the damaged intestine during surgery
- Pain around the anus or abdomen after the operation, may be treated by administration of pain-relieving drugs
- Tear at the stoma site due to local inflammation, impingement on the wound by stool, incomplete skin closure, and external pressure from a bag/stool.
- Infections because of contamination of the stoma tract with stool, increased secretion in the wound at the stoma site, and opening from the intestine to the skin surface.


Nursing Diagnosis for Colostomy
There are specific nursing diagnoses related to colostomy depending on the type of surgery, stage of recovery and other impacts that may affect the patient’s health.
The following nursing diagnoses include:
- Potential Alteration in Nutrition: This diagnosis refers to decreased intake or absorption of nutrients due to lifestyle changes, physical limitations and pain after surgery.
- Patient Education: This nursing diagnosis refers to insufficient knowledge or skills to provide care for the wound and prevent complications.
- Potential Alteration in Fluid Volume: This diagnosis refers to decreased fluid intake, stool shifts that result in dehydration or fecal impaction around the stoma.
- Abdominal distension due to gas accumulation around the stoma
- Anxiety-related to the surgery, existing condition and life changes, role transition
- Surgical site infection may affect the general health of the patient.
- Potential for Impaired Skin Integrity: This diagnosis refers to potential skin breakdown and other skin related complications after surgery due to the presence of stool around the stoma or at the opening from the intestine.
- Risk for Injury: This nursing diagnosis refers to the risk of injury from fecal impaction around the stoma or at the opening from the intestine to the skin surface.
- Dyspnea related to pain after surgery and weakness due to fatigue.
- Chronic pain that may affect the general health of the patient due to injury inflicted on the colon, rectum and anus during operation
- Constipation: This diagnosis refers to decreased bowel movements caused by inadequate fibre intake, inadequate water intake, and stool impaction around the stoma
- Risk for Infection: This diagnosis refers to infection of the wound due to fecal matter that may enter the wound or moisture accumulated at the opening from the intestine to the skin surface.
Nursing Care Plan for Colostomy
Nursing care for colostomy should focus on the following:
Monitoring vital signs, pain response and skin condition around the stoma
Educating patients about medication prescribed for wounds and prevention of further complications
Keeping good posture to avoid pressure from fecal accumulation at the opening from the intestine to the skin surface
Educating patient to lift stoma and place stool in the toilet bowl, avoid straining during bowel movement
Monitoring of fluid intake and output to prevent dehydration
Draping the stoma with clean dressing when not undergoing surgery for at least three days following surgery. A trained health care professional should do draping to avoid infection and contamination of the wound.
By following these guidelines for nursing care for colostomy, complications can be prevented, and life after surgery becomes better.


Procedure for Colostomy
Several procedures may be done depending on the type of colostomy.
Procedure for a temporary colostomy
This procedure is done to divert stool away from damaged bowel due to surgery. The surgeon will create a stoma at the level of the colon, remove a section of healthy bowel and seal the remaining open ends. The length of a temporary colostomy depends on the length of the remaining bowel. The stoma will be sealed from about 4-12 inches below the exit site. The goal is to avoid stool impaction at the opening from the intestine to the skin surface and to promote the healing of the wound.
Deciding how long you need a temporary stoma should be based on your lifestyle, strength and available support from family or friends. If you have strong supportive people around you who can help with the care of your bowel incontinence after surgery, you may not need a long-term colostomy.
Potential complications of temporary colostomy are infection at the site of an open wound, skin breakdown and accumulation of stool at the opening from the intestine to the skin surface.
Procedure for permanent colostomy
This procedure is done when the damaged bowel cannot be restored after surgery, as in the case of colon cancer. In this procedure, the surgeon will create a stoma at the level of the damaged section of the colon and rectum and then staple or suture the remaining ends together. The stoma will be sealed from about 4-12 inches below the exit site. The goal is to divert stool away from the damaged area and prevent the accumulation of stool at the opening from the intestine to the skin surface.
Potential complications for permanent colostomy are infection at the site of an open wound, skin breakdown, stomal stenosis (stoma narrows and cannot pass stool) and fecal accumulation at the opening from the intestine to the skin surface.
Bowel Technique
This is a specific technique for undertaking a colostomy. The aim is to prevent fecal matter from leaking out of the stoma. This technique helps reduce pain, swelling and other complications after surgery.
The bowel technique procedure has a low risk of complications.
Steps for bowel technique
- The patient should lie on his left side with knees bent and hips flexed towards the chest, right arm overhead in a semi-flexed position.
- The nurse will hold the stoma and ask the patient to relax while the nurse wraps a thick gauze bandage around the waist.
- The patient should remain in this position for 20 minutes.
- The next step will be to perform a bowel evacuation and irrigation of the stoma with saline solution or hydrogen peroxide solution (3%).
- The next thing to do will be to clean the entire skin area with soap and water. This procedure must be repeated every 6 hours for the first 2 days following surgery.
- The nurse will then have to apply a layer of gauze to the stoma and cover it with adhesive tape or skin prep solution. Band-Aids are not recommended as they stick to wound tissue and may cause pain, bleeding, infections and skin breakdown at the site of bandage attachment.
- Two days after surgery, the nurse will remove adhesive tape and gauze bandage and attach a wafer dressing or stoma guard. This is to prevent pressure sores from forming around the stoma.
- On day three following surgery, the nurse will remove the wafer dressing or stoma guard and apply a layer of gauze on the stoma and cover it with an adhesive bandage.
- Every day after surgery, the nurse will clean the entire skin area with a mild soap solution. About 10 days following surgery, a permanent wafer dressing or stoma guard will be applied to the stoma.
- The frequency of bowel eliminations after surgery is to follow the doctor’s orders, usually every 2-3 days until healing occurs. This will be reduced to 2 times weekly for some time.
Stomal expansion may also occur. This means that a small thin skin layer around the stoma gradually turns into a thick fold of skin. This will cause the stoma to enlarge and may cause difficulty when passing stool through that stoma opening.
Stomal enlargement is common in people who have had a colostomy for more than three months. In this case, applying an elastic ring at the base of the stoma helps keep it snugly in place. The elastic ring is applied to the stoma by a nurse and must be worn for at least two weeks continuously, followed by another two weeks with breaks of one day.
Colostomy Preoperative Measures
Explain colostomy, including the purpose of surgery, location, appearance and length of time you need a stoma.
Check the strength of your support system and if additional help is needed for colostomy care.
Discuss with the surgeon the type of colostomy procedure that is best for you and your situation.
Make an informed decision on the length of time you need a permanent stoma and type of colostomy that would be appropriate based on your lifestyle, strength and existing support system.
If the stoma is placed close to the rectum or near genitals, talk to the surgeon about the potential life-changing impacts this colostomy may have on your life.
Preparing for a colostomy (at home)
Preparation will depend on the type of colostomy you get:
If you will receive a temporary colostomy for fecal diversion, take baths, and keep the area clean and dry until surgery. If you will receive a permanent colostomy, follow instructions from the physician and dietitian for bowel preparation:
If passing large amounts of discoloured liquid stool (bowel prep), drink plenty of water to flush out your system. Use laxatives as directed. Do not eat solid food for 24 hours before surgery.
Complete the care plan as you learn more about your surgery.
Postoperative Colostomy Nursing Care Plan Measures
After the procedure, there might arise postoperative complications that include but are not limited to:
- Infection at the incision site
- Skin breakdown around wound, discoloration or oozing from stoma (when present) and accumulation of stool at the opening from the intestine to the skin surface.
- Blood in the stool occurs when the belly area had been cut. This is a common problem immediately after surgery but usually resolves on its own.
- Fecal impaction is when stool cannot be passed through the stoma because of blockage at the opening from the intestine to the skin surface. Skin breakdown around the belly and accumulation of stool at opening contributes to fecal impaction. If you suspect that you have fecal impaction, talk to your surgeon about resolving this problem.
Care plan for postoperative colostomy and the risk reduction measures:
If the patient has a Temporary Colostomy, the care plan will follow general principles of bowel care and incontinence management.
- The patient will need to be taught how to rinse the stoma as well as clean the opening from the intestine to the skin surface. The surgeon can advise on the type of irrigation and products for cleansing (e.g., bar soap, povidone-iodine solution, etc.).
- Due to the location of a stoma on the abdomen, the patient may have difficulty with body image. A plastic mirror can be used to help visualize appearance (e.g., abdominal swelling due to fecal impaction).
- Support groups for incontinence and colostomy patients may help to normalize body image.
- A fecal collection device (e.g., pouch) may be used for colostomy to collect stool that might accumulate at the opening from the intestine to skin surface if the patient does not pass stool frequently enough or when circumstances such as bowel impaction prevent the evacuation of stool from the colon.
- The patient’s diet should be encouraged to include fibre-rich foods and fluids (e.g., fruits, vegetables, whole grains, legumes) in an effort to maintain a soft stool so it may pass through the colostomy with ease. In addition, fibre supplements might be prescribed by a physician if the schedule of fibre-rich food consumption is difficult to follow.
- The patient will learn about bowel management techniques (e.g., intermittent self-catheterization) and the type of colostomy care products that are recommended for their situation (e.g., lubricant ointment, irrigation solution).
- The patient can be taught fiber supplement recommendations to promote soft stool consistency as well as what fiber-rich foods to eat at what portion sizes.
These recommendations are based on the patient’s dietitian’s prescription and the amount of time in between colostomy irrigation sessions. For example, suppose a patient is prescribed 24 ounces of fiber supplement twice per day and irrigates their colostomy once before lunch and once before dinner. In that case, they may have up to two bowel movements in between his irrigations.
For a Permanent Colostomy, care and incontinence management would be:
- The patient can be instructed to clean the opening from the intestine to the skin surface with soap and water.
- For irrigation, the patient will need a special appliance (e.g., syringe) that includes a needle or catheter for drainage of stool away from the stoma site. The recommendation is usually based on the patient’s dietitian’s prescription and the amount of time the patient can go between irrigations.
- For a colostomy that drains mucous, saline-moistened gauze may be placed over the opening to absorb fluids. Gauze should be changed every two hours or sooner if soiled. If the discharge is blood-tinged, a product called Burow’s solution is recommended. Burow’s solution may be purchased over-the-counter (e.g., Walgreens, CVS).
- The patient should try to maintain a soft stool consistency.
- If the patient does not pass fecal matter frequently enough and when circumstances such as bowel impaction prevent the evacuation of stool from the colon, a collection device may be used to collect stool that might accumulate at the opening from the intestine.
- The recommendation for diet includes fiber-rich foods and fluids (e.g., fruits, vegetables, whole grains, legumes) in order to maintain a soft stool consistency. In addition, a physician might recommend fibre supplements if the schedule of consuming a fiber-rich food is difficult to follow.
- The patient can be taught bowel management techniques (e.g., intermittent self-catheterization) and the type of colostomy products that are recommended for their situation (e.g., lubricant ointment, irrigation solution).
Nursing Interventions for Colostomy
Colostomy irrigation is advised by the dietitian to be done at a frequency of 3 times per day in some cases, and 2 times per day in others. Depending on the type of colostomy created, irrigation can be done with either saline or water solution.
The colostomy wound site should be cleaned with antibacterial soap and water prior to each irrigation session. The amount of fluid to be drained depends on the length of time between irrigations or the degree of diarrhea present.
Saline solution is recommended for a return (loop) type colostomy rather than tap water for its antibacterial action.
After irrigation, saline solution is used to clean the colostomy opening and surrounding skin surface.
After cleaning, a wafer-like dressing (e.g., Tegaderm) may be applied directly over the top of the wound opening for a permanent colostomy site. If gauze dressing is being used, it should be applied in such a way that an air hole is left open to prevent skin breakdown from continuous pressure.
A collection device may be needed for patients when bowel movements are infrequent or when circumstances such as the need to pass stool from the colon prevent the evacuation of stool.
Patient respiration should be checked for 15 seconds after each irrigation session to prevent fluid from entering the lungs.
The patient needs to understand that their dietitian may prescribe 24 ounces of specific fibre supplement(s) twice per day. This will depend on the amount and consistency of stool passed and the time between irrigation comes.
Colostomy Diet
A patient with a colostomy, often have difficulty getting enough fibre into their diet.
If the patient does not pass stool frequently enough and when circumstances such as bowel impaction prevent the evacuation of stool from the colon, a collection device may be needed for patients to collect stool that might accumulate at the opening from the intestine. The type of colostomy products that are recommended for their situation depends on the type of colostomy present.
The patient should be told to not irrigate too often as this could irritate, leading to cracks and skin breakdown. If the wound is oozing blood or leaking fluid, there is an open area in the body wall. The collection device was likely inserted incorrectly.
You may be interested in Comprehensive Nursing Diagnosis for Heart Failure
Living with Colostomy
The patient is advised to drink lots of water. This will help with bowel movements and prevent constipation.
Adjusting to this may be challenging for patients, but it is something that they learn to live with easily. You can continue doing the activities you love doing.